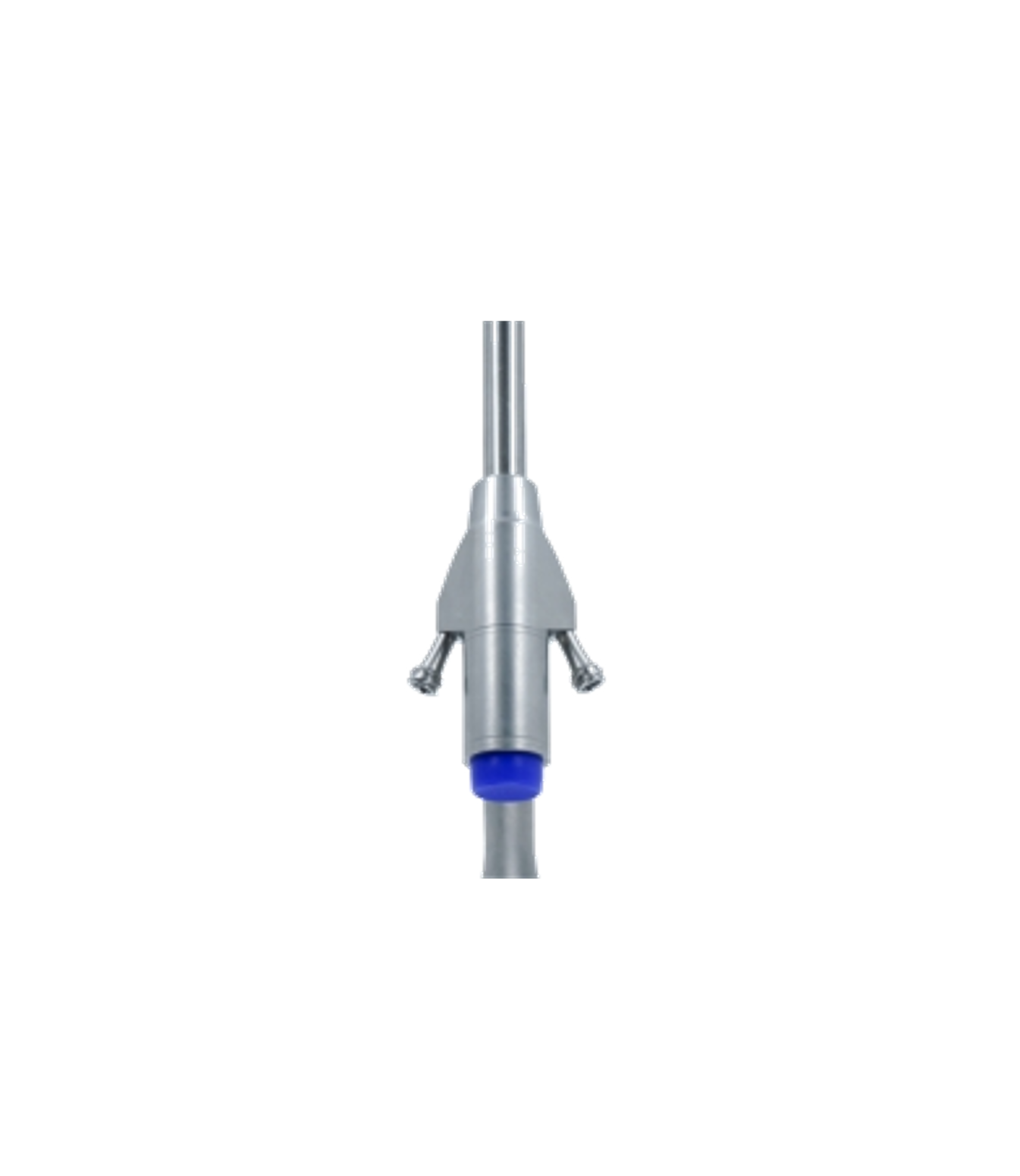
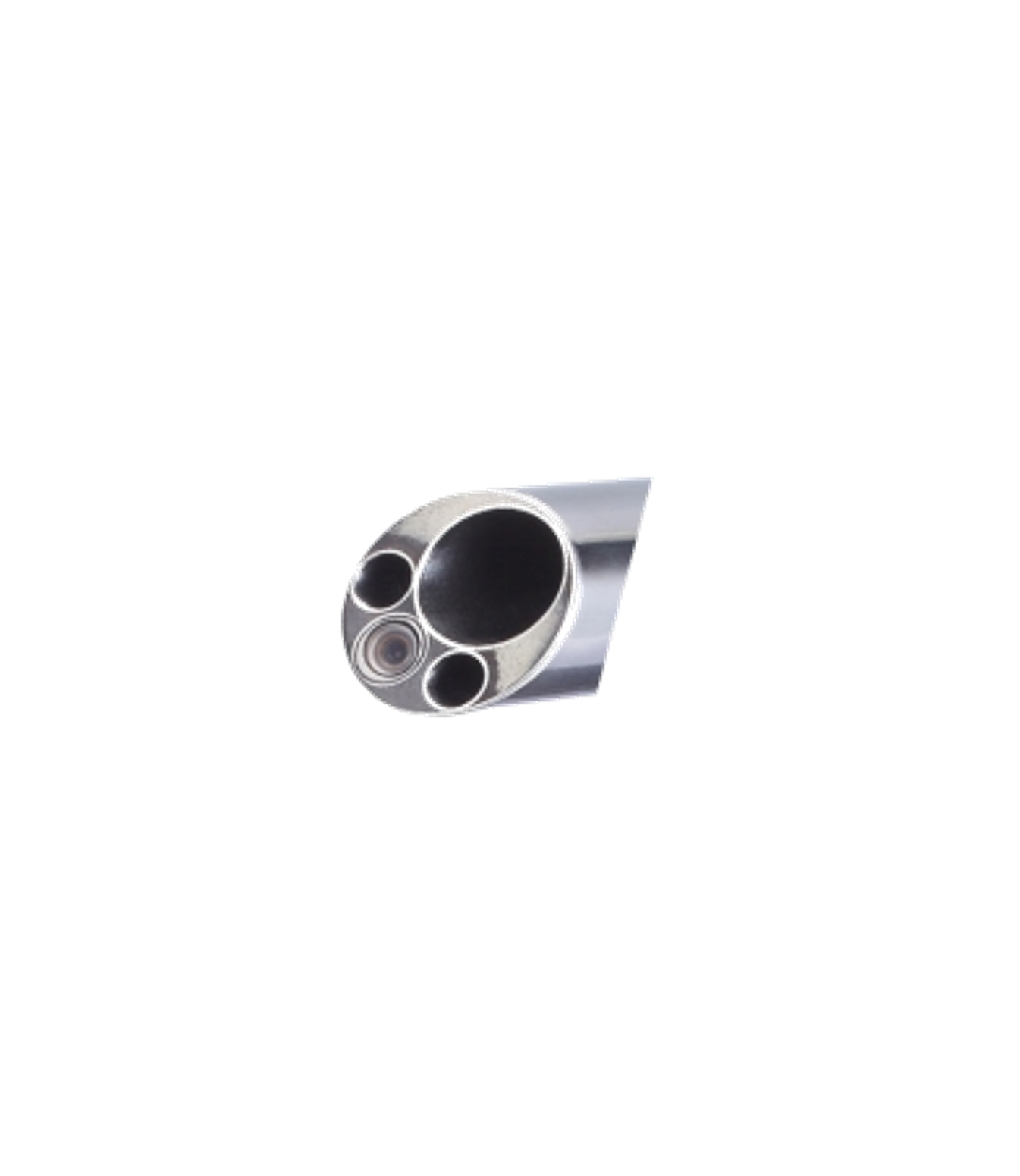
• Small trauma and less bleeding The operation is performed through a working channel with a diameter of about 7 mm, and the skin incision is usually less than 1 cm, which avoids extensive stripping of the muscles and bone structures of the lower back, thereby significantly reducing intraoperative blood loss and tissue damage, and resulting in less postoperative pain.
• Fast recovery and short hospitalization time. Most patients can get out of bed within 24 to 72 hours after surgery. The average hospitalization time is shortened to 1 to 3 days. The recovery period is shortened by more than 50% compared with traditional surgery. Daily light physical activities can usually be resumed in 2 to 4 weeks.
• Precise decompression visualization operation is guided by endoscopic magnification and image navigation. The operation can clearly identify the nerve root and dural sac, accurately remove the herniated nucleus pulposus, and the decompression accuracy exceeds 95%. It is especially suitable for difficult cases such as extreme lateral or free herniation.
• It is highly safe and has fewer complications. Local anesthesia is used to reduce systemic risks. Patients can receive real-time feedback during the operation to avoid neurovascular damage. It has less bleeding, infection probability is less than 1%, and the risk of nerve root damage is less than 0.5%. It does not damage the posterior column structure of the spine, effectively maintains stability, and reduces long-term problems such as intervertebral space collapse or adjacent segment degeneration.
• Little impact on spinal stability. Wide indications: The surgery preserves the main ligaments and bony supports of the lumbar spine to avoid paravertebral muscle atrophy. It is also suitable for symptoms such as inclusive and free disc herniation, mild spinal stenosis and other symptoms.